Personalized medicine in the treatment of acute myeloid leukemia
Acute myeloid leukemia (AML) is a highly aggressive blood disorder characterized by uncontrolled proliferation and differentiation of hematopoietic progenitor cells. AML has long been considered incurable and the majority of patients die within months of diagnosis. A personalized approach to treating this disease has given many patients hope for life.
The use of a combination of cytarabine and anthracycline antibiotics (7+3 regimen), approved by the FDA in 1973, achieved remission in more than half of patients. In 1998, intensive regimens of high-dose cytarabine were proposed to consolidate and prolong remission. For a long time, chemotherapy regimens remained unchanged. However, long-term results were poor due to the high relapse rate and the inability to use standard chemotherapy in elderly patients and those with comorbidities.
Advances in molecular biology have helped to identify a large number of genetic abnormalities in tumor cells and to characterize AML as a highly heterogeneous disease. Modern diagnostic methods make it possible to analyze the molecular profile of each patient and, based on the results, to personalize the therapeutic approach. For example, if certain mutations are detected, it is possible to use targeted drugs, while a certain number of unfavorable genetic abnormalities require allogeneic bone marrow transplantation (alloBMT).
The Immuno-Oncology Research Department of the WCRC for Personalized Medicine carries out molecular genetic studies using advanced technologies in close collaboration with the Department of Chemotherapy and Bone Marrow Transplantation of Almazov Centre. High-throughput sequencing of bone marrow samples from 20 patients with newly diagnosed AML performed in 2023 allowed to characterize in detail the characteristics of the tumor clone and to detect a high frequency of mutations in genes - regulators of the RAS-MEPK pathway (NRAS, KRAS, NF1), chromatin modifiers (KMT2C/D, DNMT3A, IDH1/2) and genes involved in DNA repair (MSH6, ATM). An increase in the total number of mutated genes and the accumulation of mutational burden during the process of clonal evolution have been shown to lead to a worse prognosis. In routine clinical practice, results on the mutational status of the FLT3 gene are available as soon as possible, allowing for timely determination of the appropriate inhibitors (midostaurin or gilteritinib). To improve the personalized approach, specialists at the Immuno-Oncology Research Department are actively investigating the prognostic value of mutations in epigenetic regulatory genes, which are frequently found in AML. The results of this study were presented at the 18 International Symposium on Acute Leukemias in Munich, Germany.
A comprehensive analysis of the patient's cytogenetic and molecular profile, as well as the monitoring of the level of minimal residual disease, allowed the formulation of specific indications for alloBMT, an immunotherapeutic method aimed at eliminating tumors by activating the graft-versus-leukemia effect.
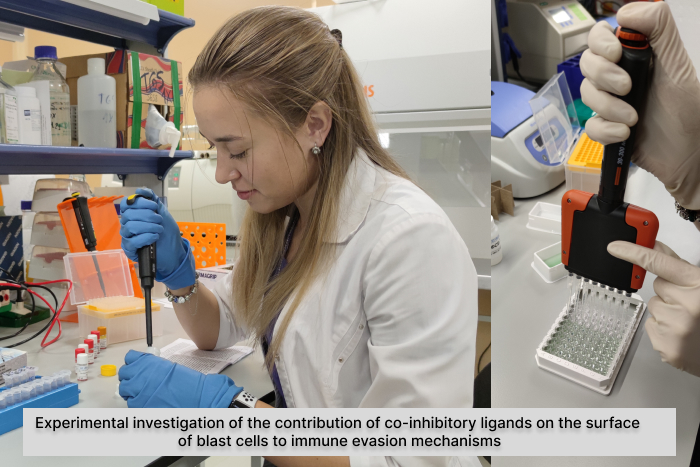
A current problem is disease relapse, which is possible even after alloBMT due to the acquired ability of the malignant clone to "escape" immune surveillance. This process is based on many mechanisms, one of which is the interaction of co-inhibitory ligands on the surface of blast cells with the corresponding T-cell receptors. Researchers at the Immuno-Oncology Research Department found that tumor cells from patients with newly diagnosed AML most frequently express the ligands CD200, CD155, galectin-9 and CD48. Detection of CD200, CD155 and galectin-9 expression is associated with poorer patient prognosis. The results were presented at the symposium entitled "Personalized immunotherapy and methods of immune response research in acute leukemia" at the 6th St. Petersburg Medical Innovation Forum.
To visualize the immunosuppressive effect, the Immuno-Oncology Research Department conducts experimental studies on cellular models.
The discovery and investigation of potential biomarkers that play a role in the escape of blast cells from the immune response will allow the identification of new potential targets for innovative targeted therapies in the future and expand the possibilities of the concept of a personalized therapeutic approach.
15.12.2023
