Results of a study on vaccination problems in children with juvenile idiopathic arthritis
Results of a study on vaccination problems in children with juvenile idiopathic arthritis
This study was carried out in the area of “Unknown, rare and genetically determined diseases”.
Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease of childhood. The main goal of JIA treatment is to control immune-mediated inflammation with various drugs (corticosteroids, methotrexate, genetically engineered biological agents). Due to abnormal immunity and the use of immunosuppressive drugs, patients with JIA are at greater risk of infections (including severe infections requiring hospitalization) than healthy children. Episodes of infection are the main reason for missing planned injections of GEBA and methotrexate with subsequent exacerbations of the underlying disease. However, many children with JIA stop vaccinating when diagnosis is established. The fear of parents and some doctors about the exacerbation of rheumatic disease often leads to the refusal of routine vaccinations. Many practicing pediatricians and pediatric rheumatologists believe that the immune response of JIA patients is impaired by immunosuppressive drugs and they do not achieve an adequate seroprotection rate.
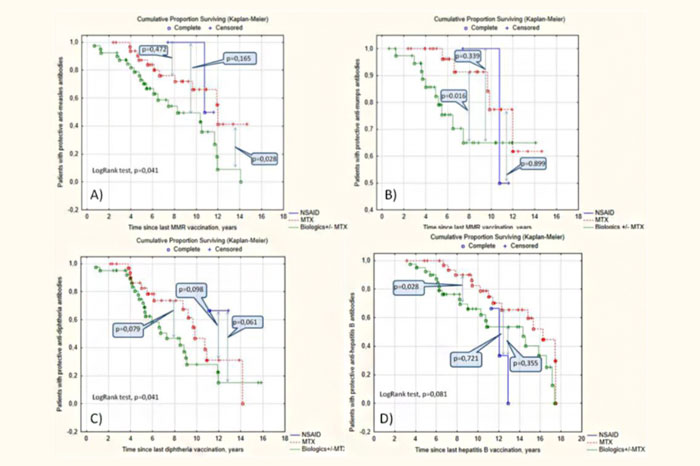
The purpose of this study was to assess vaccination coverage against measles, mumps, rubella, hepatitis B and diphtheria in a group of children with JIA; measure their post-vaccination immunity levels; identify risk factors for aberrant post-vaccination immunity in the study group.
The cross-sectional study included 170 children with various forms of juvenile idiopathic arthritis, a thorough analysis of their medical records was performed, including demographic characteristics, the course of the disease, current immunosuppressive therapy, vaccination schedule. The level of post-vaccination antibodies in the study group was measured by ELISA assays. A large amount of literature data was analyzed.
A detailed statistical analysis of the data obtained concluded that patients in the study group had a reduced level of post-vaccination antibodies. Risk factors for aberrant post-vaccination immunity are presumably both the autoimmune disease and the use of immunosuppressive drugs, as well as withdrawals from routine vaccination (including unreasonable ones). At the same time, revaccination of patients with a reduced level of post-vaccination antibodies is recognized as both effective and safe. Patients with JIA without protective levels of antibodies require routine monitoring of their levels, as well as an individual vaccination schedule.
Publication link: https://pubmed.ncbi.nlm.nih.gov/34225748/
16.07.2021
